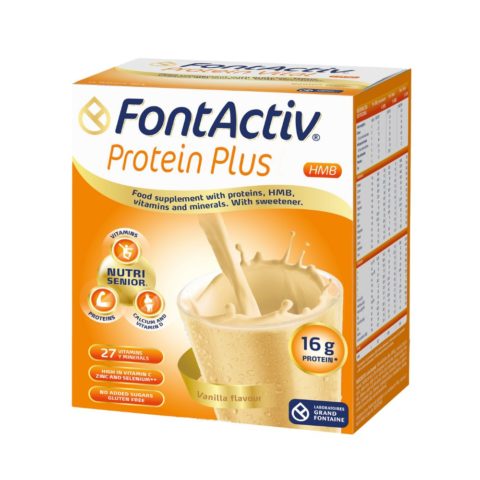
FontActiv Protein Plus
Nutritional powder solution with highly-digestible proteins and micronutrients

Joint and bone disorders encompass a wide range of conditions affecting the skeletal system, including bones, joints, ligaments, tendons, and muscles. These disorders may involve structural abnormalities, inflammation, degeneration, or trauma, leading to pain, stiffness, swelling, decreased range of motion, and functional impairment.
The most prevalent joint and bone disorders include osteoarthritis and osteoporosis. Osteoarthritis develops as the protective cartilage in the joints wears down gradually over time, causing bones to rub against each other and resulting in swelling and stiffness. On the other hand, osteoporosis is a progressive systemic skeletal disease characterized by low bone mass, leading to increased bone fragility and fracture risk. It is considered a silent condition, as it typically presents no symptoms until the occurrence of the initial fracture (1,2).
Due to population growth and ageing, there has been a rapid increase in the number of individuals experiencing musculoskeletal conditions and related functional limitations. Globally, an estimated 1.71 billion people are affected by these conditions (1).
Musculoskeletal conditions significantly limit mobility and dexterity, potentially leading to early retirement, decreased well-being, and reduced societal participation. This can contribute to additional health issues and negatively impact quality of life. Comprehensive management is essential to minimize their impact and promote healthy and active aging (1,2,3).
Oral nutrition supplements are an essential tool in the management of patients with joint and bone disorders. It has been reported that nutrients such as vitamin D and collagen are effective in treating these conditions. Vitamin D, together with calcium, is essential to prevent bone loss and reduce the risk of fracture, especially in older people. On the other hand, oral hydrolyzed collagen has been shown to reduce pain in osteoarthritis and improve chondrocyte function. These supplements are important tools to improve joint and bone health and prevent complications associated with bone loss (3,4,5,7).
Joint and bone conditions affect various demographic groups. While the prevalence of musculoskeletal conditions increases with age, younger people are also affected, often during their peak income-earning years. For example, childhood auto-immune inflammatory conditions such as juvenile arthritis affect children’s development, while low back pain is the main reason for a premature exit from the workforce (1,2).
Estrogens are responsible for the activation of fibroblast cells, the cells that produce collagen – the most abundant protein in the human body. Throughout peri-menopause and menopause estrogen levels decrease, leading to a diminution in collagen synthesis. At the onset of menopause collagen levels decline rapidly, with a reduction of 30% in the first 5 years, followed by a further decline of 2% per year for the next 15 years. Collagen is crucial in the development of osteoblast cells, cells that promote bone renewal, and stimulates the synthesis of cartilage matrix, reducing joint pain and inflammation (6).
In addition to collagen and vitamin D, other important nutrients for joint and bone health in patients with musculoskeletal disorders include hyaluronic acid and micronutrients such as vitamin C, calcium, and magnesium. These nutrients play crucial roles in strengthening cartilage regeneration and promoting bone mineralization (3,4).