
FontFast
Nutritionally complete formula high in protein and fibre for patients receiving GLP-1 therapy
Excess weight, including both overweight and obesity, can have significant effects on health. Overweight is defined as having a body weight that exceeds what is considered healthy for a given height. This condition is commonly assessed using the Body Mass Index (BMI), where a BMI between 25 and 29.9 is classified as overweight. Obesity, on the other hand, is a chronic condition characterized by the excessive accumulation of body fat, which poses a risk to health. Obesity is also commonly assessed using BMI, with a BMI of 30 or higher indicating obesity.
Both conditions increase the risk of developing diseases such as type 2 diabetes, cardiovascular problems, hypertension, bone health issues, and certain cancers. Additionally, they can affect daily activities, including sleep and mobility, ultimately reducing overall quality of life.(1-3)
Moreover, these conditions have emerged as a global health crisis, spreading rapidly across all regions and demographic groups. According to the World Health Organization (WHO), approximately 43% of the adult population is overweight, and 13% are obese. Alarmingly, it is estimated that the prevalence of obesity will rise to 24% by 2035.(4,5)
The primary intervention in the management of overweight and obesity has traditionally focused on lifestyle modifications, including dietary interventions and structured physical activity plans. However, in recent years, glucagon-like peptide-1 receptor agonists (GLP-1 RAs) have emerged as a groundbreaking innovation in obesity treatment, revolutionizing the approach to weight management.(6,7)
These medications play a critical role in regulating appetite and digestion by slowing down gastric emptying, which prolongs the sensation of fullness and naturally reduces appetite. This offers a new solution for patients who struggle with traditional weight loss methods. Clinical studies have shown that GLP-1 RA therapy can result in overall weight losses of 15% or more.(7,8)
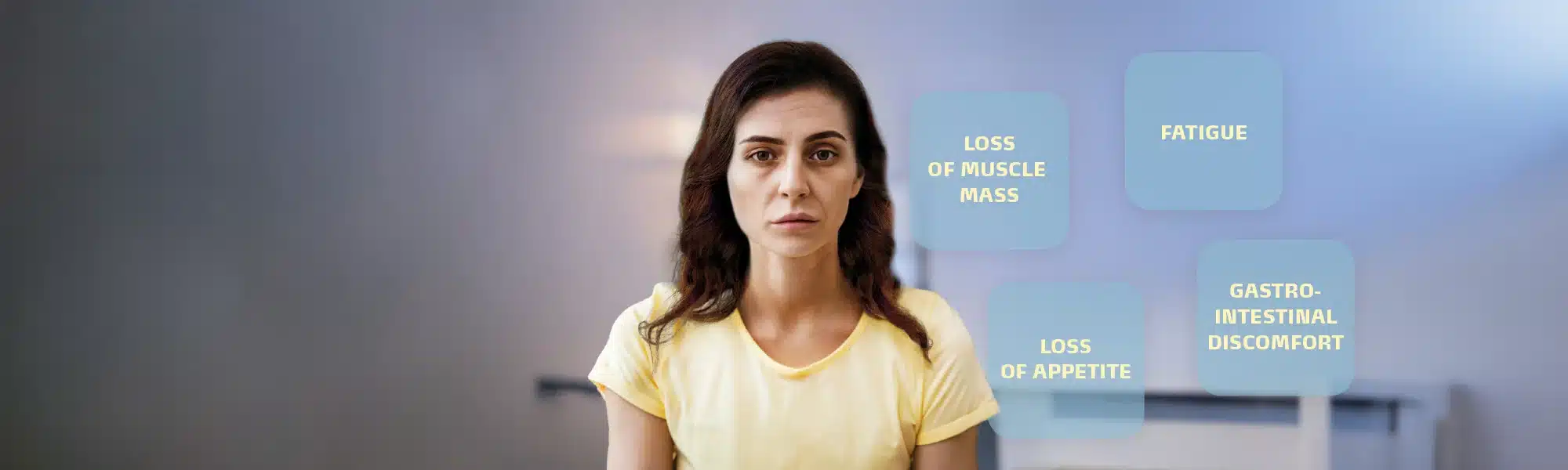
Although GLP-1 RA therapy facilitates significant weight loss and improves overall health, it is associated with potential side effects:
To avoid these side effects, it is crucial to ensure that patients’ nutritional needs are fully met through a well-balanced diet. This is particularly important to prevent the loss of muscle mass and to address deficiencies in micronutrients and other essential nutrients.
During GLP-1 therapy, the ideal diet should focus on optimizing weight loss outcomes and preventing potential side effects. It should be high in protein to preserve muscle mass, rich in fiber to manage gastrointestinal issues, and provide vitamins and minerals to avoid nutritional deficiencies. Additionally, it should ensure adequate caloric intake to maintain energy levels while supporting weight loss.
Loss of muscle mass is a significant concern during the weight loss process. This issue is particularly acute in individuals undergoing GLP-1 RA therapy who often experience a reduction in appetite, which can lead to insufficient protein consumption. Additionally, those adhering to diets with a substantial caloric deficit are at risk, as inadequate calorie intake can prompt the body to break down muscle tissue for energy. Or bariatric surgery patients, who may struggle with adequate protein intake due to reduced stomach capacity. To prevent this, adequate quality protein intake and resistance training work synergistically to effectively help preserve and build muscle mass.
GLP-1 RA medications can influence nutritional intake by reducing appetite and food consumption. Studies have shown that combining GLP-1 RA medications with meal replacement products can enhance the effectiveness of weight loss. Meal replacements are specifically designed to substitute a full meal, providing a controlled number of calories, macronutrients, and micronutrients to support weight management. These products offer a nutritionally complete option, high in protein and fibre, in a small volume, making them ideal for patients who feel satiated, thereby reducing the risk of nutrient deficiencies.
1. International Classification of Diseases 11 (ICD-11): https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/149403041
2. Alqahtani, Aayed R.; Elahmedi, Mohamed; Qahtani, Awadh A.. Prevalence of overweight and obesity in the Saudi population: A population-based cross-sectional study. Saudi Journal of Obesity 7(1):p 29-37, Jan–Jun 2019. | DOI: 10.4103/sjo.SJO_6_22.
3. Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009 Mar 25;9:88. doi: 10.1186/1471-2458-9-88. PMID: 19320986; PMCID: PMC2667420.
4. WHO 2024 https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight.
5. World Obesity Atlas 2023 https://data.worldobesity.org/publications/WOF-Obesity-Atlas-V5.pdf
6. Melson E, Ashraf U, Papamargaritis D, Davies MJ. What is the pipeline for future medications for obesity? Int J Obes (Lond). 2024 Feb 1. doi: 10.1038/s41366-024-01473-y. Epub ahead of print. PMID: 38302593.
7. Prado CM, Phillips SM, Gonzalez MC, Heymsfield SB. Muscle matters: the effects of medically induced weight loss on skeletal muscle. Lancet Diabetes Endocrinol. 2024 Nov;12(11):785-787. doi: 10.1016/S2213-8587(24)00272-9. Epub 2024 Sep 9. PMID: 39265590.
8. Christensen S, Robinson K, Thomas S, Williams DR. Dietary intake by patients taking GLP-1 and dual GIP/GLP-1 receptor agonists: A narrative review and discussion of research needs. Obes Pillars. 2024 Jul 25;11:100121. doi: 10.1016/j.obpill.2024.100121. PMID: 39175746; PMCID: PMC11340591.
9. Neeland IJ, Linge J, Birkenfeld AL. Changes in lean body mass with glucagon-like peptide-1-based therapies and mitigation strategies. Diabetes Obes Metab. 2024 Sep;26 Suppl 4:16-27. doi: 10.1111/dom.15728. Epub 2024 Jun 27. PMID: 38937282
10. Wadden TA, Chao AM, Moore M, Tronieri JS, Gilden A, Amaro A, Leonard S, Jakicic JM. The Role of Lifestyle Modification with Second-Generation Anti-obesity Medications: Comparisons, Questions, and Clinical Opportunities. Curr Obes Rep. 2023 Dec;12(4):453-473. doi: 10.1007/s13679-023-00534-z. Epub 2023 Dec 2. PMID: 38041774; PMCID: PMC10748770.
11. Gorgojo-Martínez JJ, Mezquita-Raya P, Carretero-Gómez J, Castro A, Cebrián-Cuenca A, de Torres-Sánchez A, García-de-Lucas MD, Núñez J, Obaya JC, Soler MJ, Górriz JL, Rubio-Herrera MÁ. Clinical Recommendations to Manage Gastrointestinal Adverse Events in Patients Treated with Glp-1 Receptor Agonists: A Multidisciplinary Expert Consensus. J Clin Med. 2022 Dec 24;12(1):145. doi: 10.3390/jcm12010145. PMID: 36614945; PMCID: PMC9821052